Understanding Teeth Sensitivity After Whitening
Teeth whitening is a popular cosmetic procedure, promising a brighter and more confident smile. However, many individuals experience teeth sensitivity after whitening. This discomfort can range from mild twinges to sharp, shooting pains, making it challenging to enjoy hot or cold foods and beverages. This article delves into the complexities of this common side effect, exploring the underlying causes and effective management strategies. Understanding why your teeth become sensitive after whitening is the first step towards finding relief and making informed decisions about your dental care. The process, while effective at enhancing aesthetics, can temporarily alter the tooth’s structure, leading to heightened sensitivity.
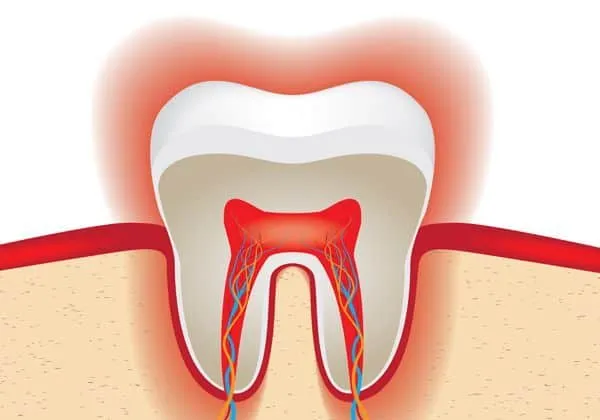
The Enamel’s Role in Sensitivity
Tooth enamel, the outermost layer of your teeth, is the hardest substance in the human body. It acts as a protective shield, insulating the sensitive inner layers from external stimuli such as temperature changes and pressure. Beneath the enamel lies dentin, which contains microscopic tubules that lead to the pulp, the tooth’s nerve center. When enamel is compromised, these tubules become more exposed, allowing stimuli to reach the nerves more easily, resulting in sensitivity. Healthy enamel is crucial for preventing sensitivity. Factors such as genetics, diet, and oral hygiene practices influence enamel health. Furthermore, the thickness of enamel varies from person to person, which explains why some individuals experience more sensitivity than others after teeth whitening procedures.
Enamel Erosion and Whitening

Whitening agents, such as hydrogen peroxide or carbamide peroxide, work by penetrating the enamel and breaking down stain molecules. While effective, these agents can also temporarily affect the enamel’s structure. They can cause minor dehydration of the enamel, making it more porous and susceptible to sensitivity. The degree of erosion depends on factors like the concentration of the whitening agent, the duration of exposure, and individual enamel characteristics. Excessive or improper use of whitening products can lead to significant enamel erosion. It’s essential to follow the instructions provided by your dentist or the product manufacturer to minimize the risk of damage and sensitivity. Maintaining proper oral hygiene, including brushing and flossing, is crucial for preserving enamel health during and after whitening treatments.
How Whitening Agents Affect the Enamel
Whitening agents work by oxidizing the stain molecules within the enamel. This process, however, can also cause a temporary loss of minerals from the enamel, making it more porous. This increased porosity allows stimuli to more easily penetrate to the dentin, causing sensitivity. The concentration of the whitening agent plays a significant role; higher concentrations can lead to more pronounced effects. The duration of exposure is also a critical factor. Prolonged exposure increases the risk of enamel damage and sensitivity. Additionally, the pH of the whitening product is important; products with a lower pH can be more acidic, potentially causing greater enamel erosion. It is very important to follow the recommendations of a dental professional when using any whitening product to minimize negative side effects.
Common Whitening Methods & Sensitivity
The method of teeth whitening can significantly influence the likelihood and severity of sensitivity. Various techniques are available, each with its unique set of advantages and potential drawbacks. Understanding these methods can help you make informed decisions and take appropriate precautions. Different whitening methods use varying concentrations of active ingredients and application durations, impacting the level of sensitivity experienced. Consulting a dentist before undergoing any whitening treatment is highly recommended to assess individual oral health and suitability for a specific method. This consultation will help to prevent future complications and maintain optimal oral health. The following sections will explore the most common methods.
In-Office Whitening

In-office whitening, performed by a dentist, typically involves a higher concentration of whitening agents, often activated by a special light. This method provides rapid results but can also lead to more intense sensitivity compared to at-home options. The dentist applies the whitening solution to the teeth, protecting the gums and soft tissues. The high concentration of the bleaching agent can penetrate the enamel more quickly, leading to quicker results. The light used in this process helps to accelerate the chemical reaction, further speeding up the whitening process. Due to the strength of the agents used, patients may experience temporary but significant sensitivity. Dentists usually provide desensitizing treatments and guidance to manage any discomfort, ensuring a safe and effective whitening experience.
At-Home Whitening Kits
At-home whitening kits offer a convenient and more gradual approach to teeth whitening. These kits often include custom-fitted trays and lower concentrations of whitening agents. This method typically results in less immediate sensitivity compared to in-office treatments, but the overall duration of treatment is longer. Patients wear the trays for a specified amount of time each day or night, as directed by their dentist. Although the concentration is lower, prolonged exposure can still cause sensitivity in some individuals. Proper use and adherence to the dentist’s instructions are crucial to minimize potential side effects. Overuse or misuse of these kits can increase the risk of sensitivity and other oral health issues. Always consult with a dentist before starting an at-home whitening regimen.
Whitening Toothpastes
Whitening toothpastes contain mild abrasive agents and sometimes low concentrations of whitening chemicals. They are designed to remove surface stains and brighten teeth over time. The abrasive nature of these toothpastes can sometimes contribute to increased sensitivity, especially if used excessively or with aggressive brushing techniques. The whitening effect is generally less dramatic than with other methods. Whitening toothpastes are more effective at preventing new stains from forming. It’s important to choose a toothpaste that is gentle on the enamel. It is recommended to consult with a dentist to determine if a whitening toothpaste is suitable for your specific oral health needs. If you experience sensitivity, consider switching to a toothpaste specifically designed for sensitive teeth.
Top 5 Causes of Sensitive Teeth After Whitening

Understanding the primary causes of sensitivity after teeth whitening can help you take preventive measures and manage any discomfort effectively. Several factors can contribute to this condition. Recognizing these causes will enable you to make informed decisions and discuss appropriate strategies with your dentist. These factors often work in combination, increasing the likelihood and intensity of sensitivity. Being aware of these elements can help in choosing the appropriate whitening method and adopting the necessary care practices to maintain oral health and a bright smile. Here’s a closer look at the top five causes.
1 Tooth Whitening Agents
The primary cause of sensitivity after teeth whitening is the whitening agents themselves, most commonly hydrogen peroxide or carbamide peroxide. These chemicals penetrate the enamel, breaking down stain molecules. This process can temporarily dehydrate the enamel, making it more porous and allowing stimuli to reach the nerves more easily. The concentration of the whitening agent is crucial; higher concentrations often lead to more significant sensitivity. The duration of exposure to these agents also affects sensitivity levels. Even with lower concentrations, prolonged use can still cause discomfort. The inherent nature of the whitening agents is to cause some level of sensitivity. The best way to mitigate the effects is to follow the instructions of your dentist or the product manufacturer.
2 Pre-Existing Sensitivity
Individuals with pre-existing sensitivity are more prone to experiencing discomfort after teeth whitening. This pre-existing sensitivity might result from various factors, including thin enamel, receding gums, or dental issues. If you already have sensitive teeth, whitening can exacerbate the condition. Thin enamel provides less protection to the underlying dentin, increasing vulnerability to sensitivity. Receding gums expose the root surfaces of teeth, which lack the protective enamel layer. Dental problems, such as cavities or cracked teeth, can also increase sensitivity. It’s essential to address any pre-existing sensitivity issues before undergoing teeth whitening. Your dentist can assess your oral health and recommend appropriate treatments to manage the sensitivity and ensure a comfortable whitening experience.
3 Improper Whitening Techniques
Improper techniques during teeth whitening can significantly increase the risk of sensitivity. This includes using excessive amounts of whitening agent, not following the instructions, or overusing the product. Applying too much whitening gel can lead to increased contact with the gums, causing irritation and sensitivity. Failing to follow the recommended duration of treatment or applying the product more frequently than advised can also contribute to sensitivity. Using ill-fitting trays that allow the whitening agent to leak onto the gums can cause irritation. Not preparing the teeth properly before whitening, such as addressing any existing dental issues, can also exacerbate sensitivity. Careful adherence to the provided instructions and consultation with a dentist are essential to prevent these issues.
4 Over-Whitening
Over-whitening, or using whitening products too frequently or for extended periods, is a common cause of sensitivity. This can occur with both in-office and at-home treatments. Overuse of the whitening agent can excessively dehydrate the enamel, making the teeth more porous and sensitive. Whitening the teeth beyond their natural shade is also a sign of over-whitening. This can result in an unnatural appearance and increase the likelihood of sensitivity. It’s crucial to follow your dentist’s recommendations and avoid the temptation to whiten more often or for longer than advised. Regular dental check-ups can help monitor your progress and prevent over-whitening. This way, the teeth can maintain their natural appearance without unnecessary discomfort.
5 Gum Irritation
Gum irritation is another significant factor contributing to teeth sensitivity after whitening. This often occurs when the whitening agent comes into contact with the soft tissues of the gums. The high concentration of the whitening agents can cause inflammation and sensitivity. Ill-fitting trays, used in at-home treatments, can allow the whitening agent to leak and irritate the gums. In-office treatments use protective measures to minimize gum contact, but sometimes, irritation still happens. If you experience gum irritation, it’s important to inform your dentist. They can provide treatments and recommend strategies to alleviate the discomfort. Avoiding contact with the gums during treatment is very important. Proper technique and the use of protective measures can minimize irritation and ensure a comfortable whitening experience.
Managing Sensitivity After Whitening

There are several effective strategies to manage sensitivity after teeth whitening and find relief. These techniques are often used in combination to provide the best possible outcome. Your dentist can recommend specific treatments tailored to your needs. Practicing good oral hygiene, and using the recommended products can help. It’s important to be patient and consistent with these methods, as it may take some time for the sensitivity to subside. With the right care, it’s very possible to enjoy the benefits of a brighter smile without the discomfort of sensitivity. Consider the following steps to manage sensitivity and improve your experience after whitening.
Choosing the Right Toothpaste
Selecting the right toothpaste can make a significant difference in managing sensitivity. Toothpastes designed for sensitive teeth are formulated to provide relief. They typically contain ingredients like potassium nitrate or stannous fluoride, which help block the nerve signals that cause sensitivity. Potassium nitrate works by calming the nerves in the teeth, reducing the sensation of pain. Stannous fluoride helps to strengthen the enamel and protect against sensitivity. These toothpastes also often have a lower abrasion level, reducing the potential for enamel erosion. Avoid toothpastes with harsh abrasives or whitening agents. Brushing gently with a soft-bristled toothbrush is important to avoid further irritation. Switching to a toothpaste specifically designed for sensitive teeth is usually the first step in managing post-whitening sensitivity.
Desensitizing Toothpastes
Desensitizing toothpastes contain active ingredients that help to block the pathways to the tooth’s nerves, reducing sensitivity. Potassium nitrate is a common ingredient, working by calming the nerve endings within the tooth. Other formulations contain stannous fluoride, which helps to strengthen the enamel and protect against external stimuli. These toothpastes typically take a few weeks of consistent use to provide noticeable relief. Brushing with a desensitizing toothpaste before and after whitening can help minimize the onset of sensitivity. Using a soft-bristled toothbrush with these toothpastes is important to avoid further enamel erosion. Always follow the instructions provided by the manufacturer for optimal results and consult your dentist if sensitivity persists.
Fluoride Treatments

Fluoride treatments, either applied at home or by a dentist, can help strengthen tooth enamel and reduce sensitivity. Fluoride remineralizes the enamel, making it more resistant to acid attacks and external stimuli. Dentists often provide professional fluoride treatments in the form of gels, varnishes, or foams. These treatments contain a higher concentration of fluoride than over-the-counter products. At-home fluoride treatments might include rinses or toothpastes with higher fluoride levels, as recommended by your dentist. Consistent use of fluoride can significantly reduce sensitivity, especially after teeth whitening. Consult your dentist for the most suitable fluoride treatment option. They will consider your individual needs and provide tailored guidance. Fluoride treatments are a proven method to protect and strengthen teeth, contributing to a healthier, less sensitive smile.
Dietary Considerations
Dietary choices play an important role in managing teeth sensitivity. Certain foods and beverages can exacerbate the discomfort, while others can provide relief. Being mindful of your diet can help minimize sensitivity and improve overall oral health. Avoiding certain foods is very important. Additionally, it’s useful to add some foods into the diet that promote oral health. Following these guidelines can reduce sensitivity.
Foods to Avoid
Certain foods and drinks can trigger or worsen teeth sensitivity. Extremely hot or cold foods and beverages are common culprits, as they can directly stimulate the sensitive nerves in the teeth. Acidic foods, such as citrus fruits, tomatoes, and vinegar, can erode enamel and increase sensitivity. Sugary foods and drinks contribute to tooth decay, which can also increase sensitivity. Sticky and chewy foods can stick to the teeth and make it harder to clean, leading to increased sensitivity. It’s advisable to avoid these items or consume them in moderation. When consuming acidic foods, it’s best to rinse your mouth with water afterward to minimize their impact on the enamel. Being mindful of your diet can significantly reduce sensitivity.
Foods to Enjoy

Incorporating certain foods into your diet can help promote oral health and reduce sensitivity. Foods rich in calcium, such as dairy products, strengthen the enamel and protect against sensitivity. Foods high in fiber, like fruits and vegetables, stimulate saliva production, which helps neutralize acids in the mouth. Water is essential for oral health, as it helps rinse away food particles and bacteria. Foods that are low in sugar and acidity are also beneficial. It’s important to maintain a balanced diet, including various nutrients that support overall health and strong teeth. Eating these foods can complement the other treatments for sensitivity.
When to See a Dentist
While many cases of teeth sensitivity after whitening are temporary and can be managed at home, it’s important to know when to seek professional dental care. If your sensitivity is severe, persists for more than a few weeks, or is accompanied by other symptoms, such as pain or swelling, it’s essential to consult your dentist. The dentist can diagnose the underlying cause of your sensitivity and recommend appropriate treatments. Persistent sensitivity can be a sign of underlying dental issues, such as cavities or gum disease. Your dentist can also determine if the whitening treatment caused any damage and provide guidance on managing the sensitivity. Regular dental check-ups are crucial for monitoring your oral health and addressing any concerns promptly.
In conclusion, experiencing sensitive teeth after whitening is a common occurrence. Understanding the causes, such as the effects of whitening agents, pre-existing sensitivity, and improper techniques, is the first step toward finding relief. Effective management strategies include using desensitizing toothpastes, fluoride treatments, and making dietary adjustments. Consulting with your dentist is crucial for personalized advice and professional care. By following these guidelines, you can enjoy the benefits of a brighter smile with minimal discomfort.
